
Au cours de mes nombreuses années d'exercice de la médecine, j'ai été le témoin direct de l'interaction complexe entre l'aide médicale à mourir (AMM) et la maladie mentale au Canada. Le débat en cours sur ce sujet a mis en lumière des questions essentielles sur l'autonomie et la vulnérabilité des patients, ainsi que sur l'état de préparation de notre système de soins de santé à l'heure où nous entrons dans un espace inconnu. Avec la changements législatifs récents et exclusion temporaire des maladies mentales Si l'on considère que l'accès à l'assurance-maladie n'est plus une condition unique d'éligibilité à l'assurance-maladie, nous nous trouvons à un moment charnière de l'histoire des soins de santé au Canada. Cet article a pour but d'analyser les nuances de ce sujet controversé, en explorant l'équilibre délicat entre le respect des choix individuels et la protection des personnes les plus vulnérables de notre société.
Situation actuelle de la MAID pour les maladies mentales au Canada
Le statut actuel de la Assistance médicale à la mort (AMM) Le traitement des maladies mentales au Canada est en pleine mutation. Les développements récents ont des implications significatives pour les patients, les prestataires de soins de santé et l'ensemble de notre système de soins de santé mentale.
Le projet de loi C-62 et l'exclusion temporaire
Projet de loi C-62qui a reçu la sanction royale en janvier 2024, a introduit une exclusion temporaire de la maladie mentale comme seule condition d'éligibilité à la MAID. Cette mesure législative a effectivement interrompu l'extension de la couverture MAID aux personnes dont la seule condition médicale est un trouble mental. La décision découle de préoccupations concernant la capacité de notre système de soins de santé à traiter de manière appropriée des cas aussi complexes.
Cette exclusion temporaire devrait rester en vigueur jusqu'au 17 mars 2027, à moins que les deux chambres du Parlement n'adoptent une résolution pour y mettre fin plus tôt. Au cours de cette période, le gouvernement entend se concentrer sur le renforcement des garanties, l'élaboration de normes de pratique claires et l'amélioration de l'accès aux soins de santé mentale dans l'ensemble du pays.
Défis liés à la mise en œuvre de la MAID pour les troubles mentaux
Le principal défi de la mise en œuvre de la MAID pour les troubles mentaux est d'identifier correctement les affections irrémédiables. En tant que personne à la pointe de l'innovation en matière de soins de santé mentale avec Field Trip, je crains qu'un nombre insuffisant de médecins ne comprennent la gamme complète des traitements disponibles pour leurs patients. De plus, le gouvernement ne subventionne pas suffisamment les traitements qui peuvent sauver la vie de nombreuses personnes souffrant de troubles mentaux.
Un autre obstacle important est la nécessité d'une formation complète et de lignes directrices pour les praticiens des soins de santé. L'évaluation de l'éligibilité à la MAID dans les cas de maladie mentale nécessite une compréhension nuancée de la maladie et des options de traitement disponibles. En l'absence d'une formation adéquate et de normes en place, il existe un risque d'application incohérente de la MAID dans les différentes régions et les différents établissements de soins de santé.
Critères d'éligibilité à la MAID dans les cas de maladie mentale au Canada
Les critères d'éligibilité à l'aide médicale à mourir (AMM) dans les cas de maladie mentale présentent des défis uniques qui nécessitent un examen approfondi. J'ai personnellement été témoin du potentiel de transformation des traitements innovants en matière de santé mentale. Je pense donc qu'il est essentiel d'aborder ces critères avec une compréhension nuancée de la complexité des troubles mentaux et de l'évolution du paysage des interventions thérapeutiques.
Définir les conditions douloureuses et irrémédiables
Le concept d'état “grave et irrémédiable” dans le contexte de la maladie mentale est particulièrement complexe. D'après mon expérience à Visite sur le terrain - Santé, Nous avons vu des patients qui étaient auparavant considérés comme résistants aux traitements répondre positivement à de nouvelles thérapies telles que la psychothérapie assistée par les psychédéliques. Cela soulève d'importantes questions sur ce qui constitue réellement un état irrémédiable dans le domaine de la santé mentale.
Par exemple, nous avions un patient souffrant d'une dépression sévère et résistante au traitement qui avait envisagé de prendre un MAID. Après avoir suivi un traitement de thérapie assistée par les psychédéliquesEn revanche, ils ont bénéficié d'un soulagement significatif de leurs symptômes et ont choisi de continuer à vivre. Ces cas soulignent l'importance d'explorer de manière exhaustive toutes les options thérapeutiques disponibles avant de conclure qu'une maladie est irrémédiable.
Évaluation de la capacité et de la prise de décision autonome
Évaluer la capacité à prendre des décisions de manière autonome chez les personnes atteintes d'une maladie mentale exige un équilibre délicat. D'une part, nous devons respecter l'autonomie des patients qui sont capables de prendre des décisions éclairées concernant leurs soins. D'autre part, nous devons veiller à ce que ces décisions ne soient pas indûment influencées par les symptômes de leur maladie mentale.
Dans ma pratique clinique, j'ai observé que la capacité d'un patient peut fluctuer au fil du temps, en particulier dans les cas de maladie mentale grave. Cette variabilité nécessite un processus d'évaluation approfondi et continu. Il est essentiel que les praticiens de santé soient bien formés à la réalisation de ces évaluations et soient conscients de l'impact potentiel des symptômes de santé mentale sur la capacité de prise de décision.
| Suicide | MAID |
| Les personnes qui pensent au suicide ne veulent pas vraiment mourir, elles veulent que la douleur de la vie prenne fin. | Accélère la mort pour les personnes en situation irrémédiable |
| Ces actes sont souvent perpétrés seuls et dans le secret, laissant les proches dans un chagrin dévastateur. | Implique une prise de décision par le personnel médical et la possibilité d'impliquer les proches. |
| Souvent violents et exécutés par des personnes qui n'entrent pas dans le système médical ou qui sont mal comprises par celui-ci. | Intervention médicale non violente |
| Avec un soutien et des soins appropriés, la guérison est possible | Le renforcement des soins palliatifs peut contribuer à alléger les souffrances des mourants |
Source : Centre canadien pour la prévention du suicide
Équilibrer l'autonomie et la vulnérabilité dans le MAID
L'intersection de l'aide médicale à mourir (AMM) et de la maladie mentale présente un paysage éthique complexe qui nécessite une navigation prudente ; il s'agit d'un équilibre délicat entre le respect de l'autonomie individuelle et la protection des personnes qui peuvent être vulnérables en raison de leur état de santé mentale.
Respecter l'autonomie du patient dans les soins de santé mentale
D'après mon expérience à Field Trip Health et dans le cadre de collaborations de recherche, le respect de l'autonomie du patient est primordial dans les soins de santé mentale. Les patients atteints de maladie mentale, comme tous les individus, ont le droit de prendre des décisions éclairées concernant leur traitement et leurs soins. Cela inclut la possibilité de considérer la MAID comme une option dans les cas graves.
Cependant, l'autonomie dans le contexte de la maladie mentale est nuancée. Nous devons veiller à ce que les patients aient accès à des informations complètes sur leur état, leur pronostic et toutes les options thérapeutiques disponibles. Cela est d'autant plus important que les thérapies de santé mentale progressent rapidement, y compris les traitements psychédéliques assistés, qui se sont révélés prometteurs pour des maladies auparavant résistantes aux traitements.
Lutte contre la vulnérabilité et la détresse sociale
Tout en respectant l'autonomie, nous devons également reconnaître la vulnérabilité inhérente qui accompagne souvent la maladie mentale. Les déterminants sociaux de la santé, tels que la pauvreté, le manque de soutien social et l'accès limité aux ressources en matière de santé mentale, peuvent avoir un impact significatif sur l'état mental d'une personne et sur sa perception des choix possibles.
Dans ma pratique clinique, j'ai pu constater que la prise en compte de ces facteurs sociaux et environnementaux peut améliorer considérablement la santé mentale et la vision de la vie d'un patient. Il est essentiel que toute considération de la MAID pour les maladies mentales comprenne une analyse des facteurs sociaux et environnementaux. une évaluation approfondie de ces facteurs de stress externes et les efforts visant à les atténuer par des interventions et des systèmes de soutien appropriés.
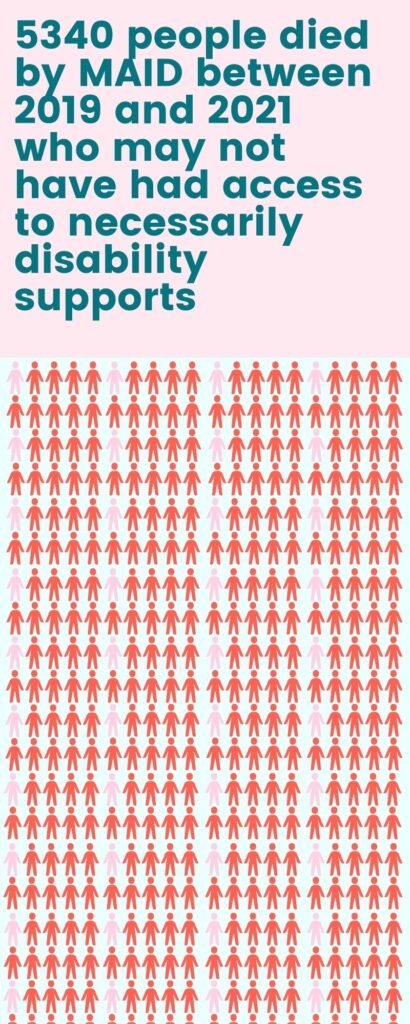
Source : Inclusions Canada Données MAID
Préparation du système de santé à la MAID et aux maladies mentales
L'état de préparation de notre système de santé à l'assistance médicale à la mort (AMM) pour les maladies mentales est une préoccupation majeure. J'ai observé des lacunes importantes dans notre système actuel qui doivent être comblées avant que nous puissions mettre en œuvre de manière responsable l'AMM pour les troubles mentaux.
Formation et lignes directrices pour les professionnels de la santé
Dans le cadre de mon travail avec des professionnels de la santé à travers le Canada, j'ai remarqué un manque inquiétant d'information sur la santé. une formation et des lignes directrices normalisées pour l'évaluation de l'éligibilité à l'AMID dans les cas de maladie mentale. De nombreux praticiens, même ceux qui ont une grande expérience de la santé mentale, ne se sentent pas préparés à faire face aux considérations éthiques et cliniques complexes que cela implique.
Pour y remédier, nous avons besoin de programmes de formation complets et nationaux qui couvrent non seulement les aspects juridiques et procéduraux de la MAID, mais aussi les nuances de l'évaluation de la santé mentale, la résistance au traitement et les thérapies émergentes. Cette formation devrait être obligatoire pour tous les prestataires de soins de santé impliqués dans les évaluations de la MAID et devrait être régulièrement mise à jour pour refléter les dernières recherches et les meilleures pratiques.
Développer les ressources et le soutien en matière de santé mentale
Un autre aspect crucial de la préparation du système de santé est le développement et l'expansion des ressources en matière de santé mentale. Grâce à mon travail à Field Trip Health et à mes collaborations avec diverses universités, il existe un énorme potentiel de transformation grâce à des thérapies innovantes telles que les traitements psychédéliques assistés. Toutefois, ces options ne sont pas encore largement disponibles ou comprises par de nombreux professionnels de la santé.
Nous devons investir dans un éventail plus large de mesures de soutien à la santé mentale, allant des thérapies traditionnelles aux traitements de pointe. Il s'agit notamment d'améliorer l'accès à la psychothérapie, de développer les programmes communautaires de santé mentale et de soutenir la recherche sur les nouveaux traitements. Ce n'est qu'en offrant une gamme complète d'options que nous pourrons faire en sorte que la MAID pour les maladies mentales au Canada soit vraiment un dernier recours.
Mesures de sauvegarde pour la MAID dans les conditions psychiatriques
Il existe un besoin vital de mesures de sauvegarde solides pour l'Assistance Médicale à Mourir (AMM) dans les conditions psychiatriques. Ces mesures sont essentielles pour protéger les personnes vulnérables tout en respectant l'autonomie de celles qui peuvent bénéficier de l'AMM en raison d'une maladie mentale grave.
Exigences de consultation et périodes d'attente au Canada
Mon expérience clinique m'a permis de constater que des consultations approfondies sont indispensables pour garantir que les demandes d'AMI dans les cas psychiatriques sont soigneusement évaluées. Ces consultations doivent impliquer plusieurs professionnels de la santé mentale, notamment des psychiatres spécialisés dans la pathologie en question. Il n'est pas rare que je collabore avec des collègues de diverses spécialités afin de bien comprendre l'état d'un patient et ses antécédents thérapeutiques.
Les périodes d'attente obligatoires sont tout aussi importantes. Elles permettent de procéder à une évaluation minutieuse et offrent la possibilité de Traitements alternatifs. Par exemple, à Field Trip Health, nous avons vu des patients qui avaient d'abord envisagé la MAID, mais qui ont trouvé que la MAID n'était pas une solution pour eux. un soulagement significatif grâce à des thérapies innovantes telles que la psychothérapie assistée par les psychédéliques pendant la période d'attente. Ces périodes permettent également de s'assurer que la décision est cohérente dans le temps et qu'elle n'est pas influencée par des facteurs temporaires ou des épisodes aigus.
Distinguer les idées suicidaires des demandes de MAID
L'un des aspects les plus difficiles de la MAID dans les conditions psychiatriques est le suivant faire la distinction entre les idées suicidaires et une véritable demande d'aide à la mort. En tant que médecin ayant traité de nombreux patients atteints de maladies mentales graves au Canada, je peux témoigner de la complexité de cette distinction. Les pensées suicidaires sont souvent un symptôme d'une maladie mentale qui peut fluctuer dans le temps et répondre à un traitement, alors qu'une demande de MAID devrait être une décision stable et mûrement réfléchie.
Pour y remédier, nous avons besoin d'outils d'évaluation complets et de lignes directrices qui aident les praticiens à faire la différence entre ces deux scénarios. Il s'agit d'évaluer la cohérence de la demande dans le temps, la compréhension par le patient de son état et du pronostic, ainsi que sa réponse aux différents traitements. Il est essentiel que nous abordions chaque cas avec empathie et rigueur, en veillant à ce que toutes les options thérapeutiques disponibles aient été explorées avant d'envisager une MAID.
Impact de la MAID sur les soins de santé mentale au Canada
L'introduction de l'assistance médicale à mourir (AMM) pour les maladies mentales au Canada a des implications considérables pour notre système de soins de santé mentale. Il est essentiel d'examiner comment l'AMM pourrait remodeler notre approche des soins de santé mentale et éventuellement apporter des améliorations à notre système actuel.
Lutter contre la stigmatisation en psychiatrie
L'introduction de la MAID pour les maladies mentales a mis au premier plan la question de la stigmatisation en psychiatrie. La stigmatisation peut avoir un impact significatif sur les soins et les résultats des patients. Le débat sur la MAID a mis en évidence la nécessité d'une compréhension plus nuancée de la maladie mentale, tant chez les professionnels de la santé que dans le grand public.
Cette attention accrue pourrait conduire à des discussions plus ouvertes sur la santé mentale, réduisant potentiellement la stigmatisation associée aux maladies psychiatriques, ce que nous espérons. C'est l'occasion d'informer les gens sur la complexité des maladies mentales et sur les différentes options de traitement disponibles, y compris les thérapies innovantes comme les traitements psychédéliques assistés que nous proposons à Field Trip Health.
Améliorer l'accès et le soutien en matière de santé mentale
Le débat sur l'AMI a également mis en lumière les lacunes de notre système de soins de santé mentale, et je pense que cela pourrait être un catalyseur pour améliorer l'accès aux ressources et au soutien en matière de santé mentale à travers le Canada. L'exclusion temporaire de la maladie mentale comme seule condition d'éligibilité à la MAID offre la possibilité de renforcer notre infrastructure de soins de santé mentale, ce qui devrait conduire à une augmentation du financement de la recherche en santé mentale, à l'expansion des programmes communautaires de santé mentale et à un meilleur accès à une gamme plus large de thérapies.
Chez Field Trip Health, nous avons constaté l'impact positif de traitements innovants tels que la psychothérapie assistée par les psychédéliques. Le débat sur la MAID pourrait accélérer l'intégration de ces nouvelles approches dans les soins de santé mentale traditionnels, offrant ainsi davantage d'options aux personnes souffrant d'affections résistantes aux traitements.
Considérations futures sur la MAID et la maladie mentale
Alors que nous envisageons l'avenir de l'assistance médicale à mourir (AMM) pour les maladies mentales au Canada, il est clair que nous entrons en territoire inconnu. Les débats en cours et les changements législatifs reflètent la complexité de cette question. Je pense qu'il est essentiel que nous abordions ces considérations futures avec un équilibre de prudence et d'ouverture d'esprit.
Examen parlementaire en cours et recommandations du groupe d'experts
Le processus d'examen parlementaire et les recommandations du groupe d'experts joueront un rôle essentiel dans l'élaboration de l'avenir de l'AMI pour les maladies mentales. L'examen en cours doit impliquer un large éventail de parties prenantes, notamment des professionnels de la santé mentale, des éthiciens, des experts juridiques et, surtout, des personnes ayant une expérience vécue de la maladie mentale.
Ces examens et recommandations devraient se concentrer sur des domaines clés tels que l'affinement des critères d'éligibilité, le renforcement des garanties et l'amélioration de l'accès aux ressources de santé mentale. Il est essentiel que ces discussions s'appuient sur les dernières recherches en matière de traitement de la santé mentale, y compris les thérapies innovantes qui se sont révélées prometteuses dans le traitement d'affections auparavant résistantes.
Évolution possible des politiques et des normes en matière de soins de santé
À mesure que nous avançons, j'anticipe des développements significatifs dans les politiques et les normes de soins de santé liées à la MAID et à la maladie mentale. Sur la base de mon travail à Field Trip Health et de mes collaborations en matière de recherche, je pense que nous assisterons à une pression en faveur de protocoles d'évaluation plus complets et normalisés pour les demandes de MAID dans les cas de maladie mentale. Ces protocoles comprendront probablement des consultations obligatoires avec plusieurs spécialistes de la santé mentale et des périodes d'observation prolongées afin de garantir une capacité de prise de décision cohérente.
En outre, je m'attends à ce que l'on mette davantage l'accent sur l'intégration des discussions sur la MAID dans les cadres plus larges des soins de santé mentale. Cela pourrait impliquer l'élaboration de nouvelles normes de pratique pour discuter des options de fin de vie avec les patients souffrant de troubles mentaux, ainsi que l'élaboration de nouvelles normes de pratique pour les patients souffrant de troubles mentaux. des lignes directrices permettant de s'assurer que toutes les options thérapeutiques ont été étudiées de manière approfondie avant d'envisager une MAID. En fin de compte, ces développements politiques devraient viser à trouver un équilibre entre le respect de l'autonomie du patient et la protection des personnes vulnérables.
Façonner l'avenir : MAID, la maladie mentale et l'évolution des politiques de santé au Canada
L'intersection de l'assistance médicale à la mort (AMM) et de la maladie mentale présente un paysage complexe qui continuera d'évoluer dans les années à venir. Alors que nous naviguons sur ce terrain difficile, il est crucial que nous maintenions un équilibre délicat entre le respect de l'autonomie individuelle et la protection des personnes les plus vulnérables. L'exclusion temporaire de la maladie mentale en tant que seule condition d'éligibilité à la couverture MAID nous offre une opportunité précieuse. Nous devons utiliser ce temps pour renforcer notre système de soins de santé mentale, développer des garanties complètes et nous assurer que toutes les options de traitement disponibles sont épuisées avant d'envisager l'adoption de la MAID.
J'ai été témoin du potentiel de transformation de nouvelles thérapies telles que la psychothérapie assistée par les psychédéliques et la stimulation magnétique transcrânienne répétitive (SMTr) et j'ai vu des patients retrouver leur vie. Ces expériences soulignent l'importance d'approfondir sans cesse notre compréhension des maladies mentales et d'explorer de nouvelles voies de traitement. À mesure que nous avançons, il est essentiel que nous restions ouverts aux nouvelles perspectives et aux recherches émergentes, car les discussions en cours autour de la MAID et des maladies mentales ont le potentiel d'entraîner des changements positifs dans notre système de soins de santé. En luttant contre la stigmatisation, en améliorant l'accès aux ressources en matière de santé mentale et en favorisant un dialogue ouvert, nous pouvons œuvrer à une approche plus compatissante et plus efficace des soins de santé mentale. Les décisions que nous prenons aujourd'hui façonneront l'avenir des soins de santé mentale au Canada. Abordons ce défi avec empathie et sagesse, et en nous engageant à assurer le bien-être de tous les Canadiens qui luttent contre la maladie mentale.
Questions fréquemment posées
En raison de préoccupations concernant les garanties adéquates et l'état de préparation du système, l'éligibilité à la MAID basée uniquement sur la maladie mentale a été reportée jusqu'en mars 2027.
Le gouvernement vise à renforcer les garanties, à améliorer l'accès aux soins de santé mentale et à élaborer des normes claires pour la MAID dans les cas de maladie mentale.
Il s'agit d'affections causant des souffrances graves et intolérables qui ne répondent à aucune option de traitement raisonnable, bien que cela soit complexe dans les cas de santé mentale.
Cet équilibre exige de respecter les choix du patient tout en veillant à ce qu'ils ne soient pas influencés par des symptômes de santé mentale traitables ou par un manque de soutien.
L'évaluation de la capacité dans les cas de maladie mentale est rigoureuse et nécessite souvent des évaluations répétées par des professionnels de la santé mentale qualifiés afin de garantir un consentement éclairé.
Avant d'envisager une MAID, tous les traitements raisonnables, y compris les options innovantes comme la thérapie assistée par les psychédéliques, doivent être explorés afin de garantir une prise en charge complète.
A propos de l'auteur

Dr. Mario Nucci MD CCFP est un médecin de famille agréé qui se passionne pour la santé mentale et le développement de nouvelles thérapies. Il est activement engagé dans la recherche avec un poste de professeur associé à l'École de médecine du Nord de l'Ontario et des collaborations de recherche avec l'Université d'Ottawa, l'Université de Calgary, l'Université Lakehead, l'Université Concordia et l'Université de l'île de Vancouver.
Le Dr Nucci est le fondateur du Bay and Algoma Health Centre en 2019, une clinique de médecine sans rendez-vous et de toxicomanie. Il a fondé le Canadian Centre for Psychedelic Healing en 2019, qui opère maintenant sous le nom de Field Trip Health, offrant des soins de santé mentale de pointe dans les régions de l'Atlantique. Toronto, Montréal, Vancouver, Ottawa, Hamilton, Kitchener-Waterloo, Thunder Bay, Sault Ste. Marieet à domicile.